TIM-3 in Alzheimer’s treatment has emerged as a groundbreaking focus in Alzheimer’s disease research, opening up new avenues for therapy. This immune checkpoint molecule, previously recognized for its role in cancer therapy, is now being investigated to enhance cognitive improvement in Alzheimer’s patients. Recent studies demonstrate that targeting TIM-3 can potentially unleash the brain’s own immune cells, known as microglia, allowing them to effectively attack and clear amyloid plaques that accumulate in the brains of those suffering from Alzheimer’s. By inhibiting TIM-3’s function, researchers aim to restore the natural cleaning processes of these immune cells, which not only reduces plaque burden but also fosters enhanced memory function. The implications of this innovative TIM-3 therapy could transform the landscape of Alzheimer’s treatment, shifting the paradigm toward harnessing the body’s own defenses to combat this debilitating disease.
The role of TIM-3 in Alzheimer’s disease intervention is gaining significant traction, particularly as researchers delve deeper into immune response mechanisms underlying neurodegeneration. As an immune checkpoint inhibitor, TIM-3 has shown promising potential in cancer therapeutics, and its application in neurological disorders is being explored. Enhanced understanding of microglial cell behavior reveals how modulation of TIM-3 can lead to improved outcomes in Alzheimer’s conditions by facilitating the phagocytosis of toxic amyloid beta plaques. This approach not only aims to reduce plaque accumulation but also targets pivotal pathways for restoring cognitive function in affected individuals. By reframing our strategies around existing immune pathways, TIM-3 presents an exciting frontier in the quest for effective solutions to Alzheimer’s disease.
Understanding TIM-3 in Alzheimer’s Disease
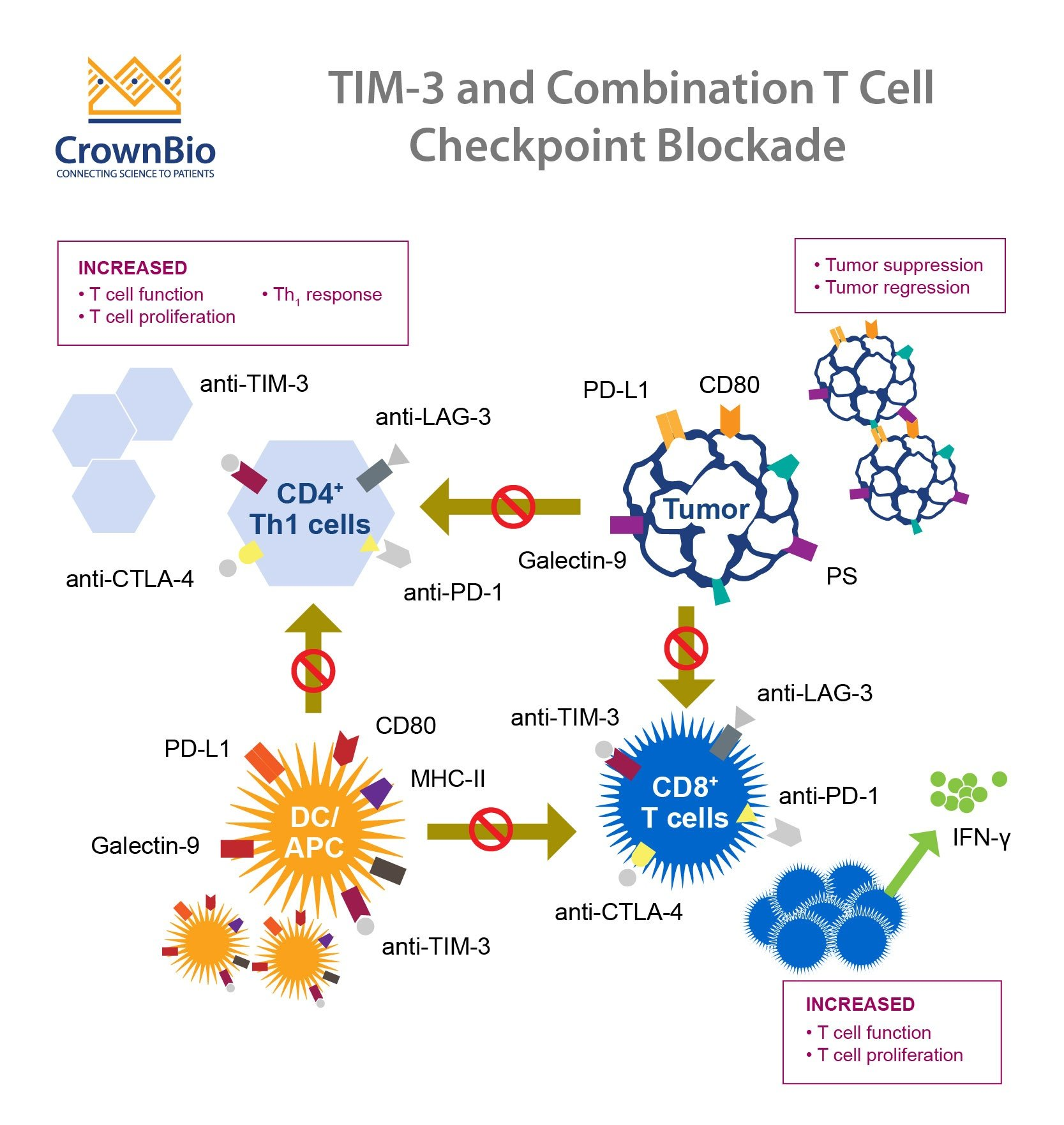
TIM-3, also known as T-cell immunoglobulin mucin-3, has emerged as a significant player in the pathology of Alzheimer’s disease (AD). This immune checkpoint molecule primarily serves to inhibit immune responses, which can prevent excessive inflammation within the brain. In a healthy system, TIM-3 regulates the activity of microglia, the brain’s resident immune cells that are crucial for clearing amyloid plaques, a hallmark of Alzheimer’s. A genome-wide association study has linked TIM-3 expression levels to late-onset Alzheimer’s, suggesting that individuals with specific polymorphisms in the TIM-3 gene may be at higher risk of developing the disease. This understanding paves the way for potential therapeutic interventions targeting TIM-3 to enhance cognitive function and mitigate Alzheimer’s progression.
Interestingly, the dual nature of TIM-3’s role complicates its application in treatment. While inhibiting TIM-3 could boost the ability of microglia to remove amyloid plaques, it also carries the risk of unleashing an uncontrolled immune response that could lead to neuroinflammation, potentially exacerbating cognitive decline. Therefore, researchers are exploring TIM-3 therapy that carefully balances enhancing immune activity while protecting neuronal integrity. By employing anti-TIM-3 antibodies, scientists hope to selectively block this inhibitory pathway, facilitating plaque clearance and promoting cognitive recovery in patients suffering from Alzheimer’s.
The Role of Microglia in Alzheimer’s Pathology
Microglia play a fundamental role in maintaining brain health by performing various functions, such as scavenging cellular debris and mediating neuroinflammatory responses. In the context of Alzheimer’s disease, these cells become dysfunctional due to the overexpression of inhibitory molecules like TIM-3. This malfunction reduces their ability to clear toxic amyloid-beta plaques, contributing to the neurodegenerative process associated with cognitive decline. Research shows that as microglia accumulate TIM-3, they shift from an active state into a homeostatic mode, becoming less capable of removing harmful substances from the brain.
Moreover, impaired microglial function leads to an accumulation of plaques, which can disrupt synaptic function and neuronal communication. This impairment is particularly pronounced in late-onset Alzheimer’s, where the burden of plaques can severely compromise cognitive abilities. Therefore, restoring the functionality of microglia by targeting TIM-3 may not only enhance their ability to clear amyloid plaques but also help improve synaptic health and cognitive function. The ongoing research into TIM-3 inhibitors is focused on harnessing this mechanism to develop effective drugs that can provide cognitive improvements in Alzheimer’s patients.
Implications of TIM-3 Therapy for Alzheimer’s Treatment
The potential for TIM-3 therapy to provide cognitive improvement in Alzheimer’s patients lies in its ability to modify the immune response within the brain. By inhibiting TIM-3, researchers aim to reactivate microglial cells, enabling them to more effectively engage with and clear amyloid-beta plaques. With promising results already seen in animal models, where the deletion of the TIM-3 gene led to plaque reduction and cognitive enhancement, TIM-3 therapy appears to be a compelling avenue for clinical development. Furthermore, this therapy could be integrated with existing Alzheimer’s treatments, enhancing their efficacy by addressing both biochemical and immune system components of the disease.
However, as with any new treatment approach, challenges remain in translating these findings into human therapies. The task of delivering anti-TIM-3 antibodies effectively to the brain among other complexities illustrates a significant hurdle. Moreover, meticulous research must confirm that enhancing immune activity does not lead to adverse inflammatory responses. Nonetheless, the ability of TIM-3 therapy to repurpose existing immunotherapy strategies from cancer treatment to address Alzheimer’s provides a robust foundation for future studies aimed at improving patient outcomes.
Recent Advances in Alzheimer’s Disease Research
Recent studies have significantly advanced our understanding of how immune checkpoint molecules like TIM-3 can reshape the landscape of Alzheimer’s disease research. As scientists explore the intricate connections between immunology and neurodegeneration, innovative therapies are emerging that target specific pathways involved in amyloid plaque formation and cognitive decline. By dissecting the molecular mechanisms that underlie Alzheimer’s pathology, the focus has shifted to creating therapeutic strategies that not only treat symptoms but also address the root causes of the disease.
Key breakthroughs have highlighted the potential to modulate microglial activity through pharmacological interventions. By utilizing TIM-3 inhibitors as a method to enhance the innate clearance mechanisms of microglia, researchers are optimistic about developing drugs that can restore memory functions in Alzheimer’s patients. This evolving field points towards a future where a multifaceted approach to Alzheimer’s treatment—combining immunotherapy with traditional pharmacological methods—could revolutionize how we address this complex and challenging disease.
How TIM-3 Therapy Can Enhance Cognitive Function
One of the most compelling benefits of TIM-3 therapy is its potential to enhance cognitive function in Alzheimer’s disease patients. Research has demonstrated that by blocking TIM-3 on microglia, these immune cells can resume their role in plaque clearance, which in turn may lead to improvements in memory and learning abilities. Improved cognitive function is not just a theoretical outcome; initial studies in mice have shown that genetically altering microglial TIM-3 expression resulted in marked improvements in cognitive tasks, suggesting a direct correlation between TIM-3 inhibition and enhanced memory.
Furthermore, cognitive improvement in Alzheimer’s is vital for quality of life, as it can impact day-to-day activities, social interactions, and overall mental health. As researchers continue to investigate TIM-3’s role, the focus is on translating these promising animal study results into human clinical trials. The ultimate goal is to establish a new standard of care for Alzheimer’s patients that integrates TIM-3 inhibitors into broader therapeutic regimens aimed at mitigating the disease’s cognitive impact.
Challenges in Developing TIM-3 Based Treatments
While the prospects for TIM-3 based treatments in Alzheimer’s disease are promising, several challenges must be addressed before such therapies can be widely implemented. Potential adverse effects associated with enhanced immune activity present a significant concern. In the human brain, an overactive immune response can lead to neuroinflammation, complicating efforts to balance effective plaque clearance with the risk of unintended inflammatory damage to healthy neurons.
Another challenge lies in the delivery mechanisms for TIM-3 inhibitors. Ensuring that these therapies can effectively penetrate the blood-brain barrier remains a critical hurdle in Alzheimer’s drug development. Continued research is required to find ways to optimize drug delivery while maintaining therapeutic efficacy. Furthermore, longitudinal studies will be needed to monitor any long-term effects of TIM-3 inhibition on neurological health, highlighting the importance of careful and comprehensive clinical trial designs to establish safety and efficacy for potential TIM-3 targeting therapies.
The Future of Neuroimmunology in Alzheimer’s Research
The integration of neuroimmunology into Alzheimer’s research has opened up new avenues for exploring how the immune system interacts with neurodegenerative processes. With increasing evidence linking immune modulation to cognitive outcomes, the future of Alzheimer’s therapies may focus heavily on understanding and manipulating immune pathways like those involving TIM-3. By advancing our comprehension of the immune system’s role in brain health, researchers are laying the groundwork for innovative treatments that could reshape Alzheimer’s management strategies.
In the coming years, as research in this dynamic field progresses, we may witness a paradigm shift where immunotherapy becomes a standard component of Alzheimer’s treatment regimens. Explorations into the connections between microglial activation, TIM-3 receptor modulation, and cognitive function will be crucial in designing targeted therapies aimed at halting or even reversing the effects of Alzheimer’s. Overall, the future for TIM-3 therapy looks bright, promising a new frontier in the pursuit of effective solutions for Alzheimer’s disease.
Exploring TIM-3 Inhibitors for Clinical Applications
As the research on TIM-3 continues to evolve, the exploration of TIM-3 inhibitors as a potential treatment for Alzheimer’s disease presents an exciting opportunity to leverage previously established cancer therapies in a new context. Clinical applications of TIM-3 inhibitors will need to be meticulously developed and adapted to ensure that they are tailored to address the unique challenges posed by Alzheimer’s pathology. This includes evaluating their safety and efficacy in human subjects and determining the optimal timing and dosing strategies to maximize therapeutic benefits.
Current investigations into TIM-3 inhibitors focus on their ability to re-activate microglia’s phagocytic functions without triggering excessive inflammation. These inhibitors may serve as a vital piece in the puzzle of Alzheimer’s treatment, particularly as researchers work to refine their approaches to ensure safe and effective applications. With promising animal model results and robust ongoing research, TIM-3 inhibitors could soon transform the landscape of Alzheimer’s treatment and represent a significant step forward in enhancing cognitive health for millions of affected individuals.
The Collaborative Efforts in Alzheimer’s Research
The complexity of Alzheimer’s disease necessitates collaborative efforts across various fields of research, highlighting the importance of interdisciplinary approaches in developing effective therapies. Teams of neurologists, immunologists, geneticists, and pharmacologists are working together to understand the nuanced interactions between amyloid pathology, microglial function, and immune system modulation. Such collaboration is crucial as it consolidates diverse expertise, ensuring that research into TIM-3 and its effects on Alzheimer’s is thorough and multidimensional.
These collaborative research efforts are gaining momentum, with institutions joining forces to pool resources and share knowledge. For instance, joint initiatives focused on TIM-3 research have the potential to accelerate the discovery of viable therapeutic options and foster innovative strategies that enhance cognitive improvement in patients with Alzheimer’s. As the field progresses, the synergy generated by these cooperative endeavors will play a pivotal role in achieving breakthroughs that may redefine our understanding and management of Alzheimer’s disease.
Frequently Asked Questions
What role does TIM-3 therapy play in Alzheimer’s disease treatment?
TIM-3 therapy targets the TIM-3 molecule, an immune checkpoint that inhibits microglia, the brain’s immune cells, from clearing amyloid plaques associated with Alzheimer’s disease. By blocking TIM-3, this therapy allows microglia to engage and eliminate these toxic plaques, potentially improving cognitive function in Alzheimer’s patients.
How does TIM-3 molecular activity affect Alzheimer’s disease progression?
TIM-3 is expressed at high levels on microglia in Alzheimer’s patients, preventing these immune cells from clearing plaque accumulation in the brain. The inhibitory role of TIM-3 limits microglial activity, leading to plaque buildup, which is a hallmark of Alzheimer’s disease and contributes to memory loss.
Can TIM-3 therapy potentially restore cognitive function in Alzheimer’s patients?
Research indicates that deleting the TIM-3 gene in mouse models of Alzheimer’s leads to improved cognitive functions by enhancing microglial clearance of amyloid plaques. While human trials are needed, TIM-3 therapy may offer a promising strategy to restore some cognitive abilities in Alzheimer’s patients.
What are microglia and how are they related to TIM-3 in Alzheimer’s disease?
Microglia are the brain’s resident immune cells that play a crucial role in clearing debris and maintaining brain health. In Alzheimer’s disease, the activity of microglia is inhibited by the TIM-3 molecule, preventing them from effectively removing harmful amyloid plaques, which can lead to cognitive decline.
What are immune checkpoint molecules, and how does TIM-3 function in this context?
Immune checkpoint molecules like TIM-3 regulate immune responses to prevent overly aggressive actions that could harm the body. In Alzheimer’s disease, TIM-3 inhibits microglial activity, preventing them from attacking amyloid plaques, which may exacerbate disease progression when functioning improperly.
What evidence supports the effectiveness of TIM-3 therapy in treating Alzheimer’s disease?
Recent studies, including those involving genetically modified mice lacking the TIM-3 gene, show that blocking TIM-3 enhances microglial plaque clearance and leads to observable cognitive improvements, pointing toward the potential effectiveness of TIM-3 therapy in Alzheimer’s treatment.
Are there any clinical trials for TIM-3 therapy in Alzheimer’s disease?
While research is promising, clinical trials for TIM-3 therapy in Alzheimer’s disease are still in early stages. Researchers are currently testing anti-TIM-3 antibodies in mouse models to evaluate their efficacy in halting plaque development and restoring cognitive functions in future human trials.
What are the future implications of TIM-3 research for Alzheimer’s disease treatment?
The future of TIM-3 research holds significant potential for Alzheimer’s treatment. As studies progress, understanding the role of TIM-3 in plaque clearance could lead to innovative therapies that target this immune checkpoint molecule, potentially providing new avenues for managing Alzheimer’s disease.
| Key Points |
|---|
| Recent research shows that TIM-3, an immune checkpoint molecule, may play a significant role in treating Alzheimer’s by enhancing microglial activity to clear brain plaques, improving cognitive functions. |
Summary
TIM-3 in Alzheimer’s treatment offers promising prospects as it may facilitate the clearance of amyloid plaques by enhancing the brain’s immune response. The recent study highlights the potential of TIM-3 blockade to improve cognition in Alzheimer’s mouse models, paving the way for innovative therapeutic approaches in tackling this challenging disease.