Microglial research is crucial in unraveling the complexities of the brain’s immune system, especially in the context of disorders like Alzheimer’s disease. These specialized cells are fundamental in maintaining brain health, as they continuously monitor, protect, and repair neural environments. Recent studies have demonstrated that dysregulation in microglial function may be a significant factor contributing to neurodegenerative diseases. This exciting scientific discovery is propelling biomedical research forward, paving the way for innovative treatments and biomarkers aimed at improving outcomes for millions of individuals affected by Alzheimer’s and related conditions. As we continue to explore the intricate roles of microglia, we may uncover transformative approaches to brain health and disease management.
Investigating the dynamics of glial cells offers profound insights into the brain’s protective mechanisms. These immune cells not only support neuronal health but also play pivotal roles in synaptic plasticity and integrity. Ongoing research into their function and interactions holds promise for understanding various neurodegenerative disorders, including Alzheimer’s disease and others affected by similar cellular dysfunctions. By deepening our grasp of these vital components of the central nervous system, researchers are unlocking novel avenues in biomedical research. Ultimately, this exploration is foundational to advancing therapeutic strategies designed to combat the devastating impact of neurodegenerative diseases.
The Role of Microglial Research in Alzheimer’s Disease
Microglial research has become pivotal in our understanding of Alzheimer’s disease and how it develops. These cells are integral to the brain’s immune system, responsible for monitoring the health of neural networks and clearing debris from the brain. As scientists delve deeper into the intricacies of microglia’s functions, including their role in synaptic pruning, it has become apparent that dysfunctions in microglial activity may lead to debilitating neurodegenerative diseases like Alzheimer’s. Beth Stevens and her team at Boston Children’s Hospital have provided critical insights into how abnormal microglial behavior contributes to synaptic loss, presenting a potential target for therapeutic intervention.
Moreover, the link between microglial dysfunction and neurodegenerative diseases underscores the importance of continued research into these immune cells. As Stevens points out, detailed studies allow researchers to understand disease mechanisms that are inaccessible in human patients. This body of knowledge is essential for the development of biomarkers and new treatment avenues. With Alzheimer’s affecting millions, advancements in microglial research hold the promise of not only elucidating disease pathways but also paving the way for innovative therapies that could improve the quality of life for those affected.
Understanding Neurodegenerative Diseases through Basic Science
The journey into understanding neurodegenerative diseases has been significantly enhanced by the principles of basic science. Researchers like Beth Stevens emphasize that foundational scientific inquiry often leads to discoveries with profound implications for human health. Without the curiosity-driven research that investigates even the most obscure areas of neurobiology, such as how microglia contribute to synaptic development, we would lack the essential knowledge required to combat diseases like Alzheimer’s. Funding from agencies like the NIH supports this critical research, enabling scientists to pursue theories that may initially seem disconnected from clinical applications.
Additionally, the translation of these basic scientific discoveries to practical treatments often follows a long and winding path. For instance, years of studying microglial cells and their functions set the stage for significant breakthroughs that could lead to innovative therapies. As Stevens notes, work that seems far removed from immediate therapeutic benefits ultimately informs our understanding of disease mechanisms. This interplay between basic research and practical outcomes is essential for developing effective treatments for Alzheimer’s and other neurodegenerative diseases, reinforcing the value of persistent scientific exploration.
The Impact of Curiosity-Driven Research on Biomedical Advances
Curiosity-driven research has long been a catalyst for scientific breakthroughs in various fields, including biomedical research. The pursuit of knowledge for its sake often leads to unexpected findings that profoundly influence our understanding of complex diseases. In the context of Alzheimer’s disease, the exploration of microglia by scientists like Beth Stevens illustrates how foundational research can lead to significant medical advances. By studying basic biological processes without immediate commercial goals, researchers can uncover essential insights that form the bedrock for future therapeutic interventions.
Furthermore, support from federal funding agencies plays an essential role in facilitating this type of research. As highlighted by Stevens, NIH-supported endeavors allow scientists to freely investigate novel ideas and hypotheses. This funding has been crucial in transforming basic research into actionable knowledge about the brain’s immune system and synaptic health. As the understanding of microglial functions evolves, so too does the potential for new treatment strategies for Alzheimer’s and other neurodegenerative diseases, revealing the profound interconnectedness of basic science and real-world medical applications.
Exploring Synaptic Pruning and Neurodegenerative Diseases
Synaptic pruning is a critical process in brain development and function, predominantly orchestrated by microglial cells. Understanding this process is essential for deciphering the pathology behind neurodegenerative diseases such as Alzheimer’s. Abnormalities in synaptic pruning, often a result of faulty microglial activity, have been linked to neurodegeneration. Researchers have found that when microglia engage in excessive or misdirected pruning of synapses, it can lead to cognitive decline and the symptoms characteristic of Alzheimer’s. Therefore, insights into synaptic pruning mechanisms are not only vital for understanding how neurodegenerative diseases develop but also for developing potential intervention strategies.
The implications of synaptic pruning extend beyond Alzheimer’s disease; they are relevant to various neurodegenerative disorders, including Huntington’s disease. The research conducted by Stevens and her colleagues emphasizes the necessity of exploring how microglial interactions affect synaptic integrity throughout the lifespan. Understanding these relationships provides a crucial framework for identifying targeted therapeutic approaches, potentially reversing or halting the progression of neurodegenerative diseases. With continued investigation into the fundamentals of synaptic pruning, there is hope for more effective treatments for those afflicted by these devastating conditions.
The Influence of Federal Funding on Alzheimer’s Research
Federal funding plays a crucial role in advancing Alzheimer’s research by providing scientists the resources necessary to pursue innovative and often exploratory avenues of inquiry. The National Institutes of Health (NIH) has been pivotal in supporting research initiatives that may not immediately promise commercially viable results. As pointed out by Beth Stevens, this funding is crucial for enabling researchers to follow promising lines of inquiry, leading to advancements in our understanding of Alzheimer’s disease and related disorders. By making significant investments in basic research, federal agencies lay the groundwork for breakthroughs that can translate into clinical applications.
Moreover, the role of funding extends beyond just providing resources; it fosters an environment of collaboration and scientific inquiry. With federal grants, researchers are encouraged to share findings and insights, creating a community of scientists focused on tackling complex problems, such as the aging brain and Alzheimer’s pathology. This collective effort emphasizes the importance of robust financial support in enhancing scientific discovery in the field of neurobiology. The contribution of federal funding is, therefore, not merely a financial consideration but a vital catalyst for progress in the fight against Alzheimer’s disease and other neurodegenerative disorders.
Advancements in Biomarkers for Alzheimer’s Disease
The search for effective biomarkers has become a cornerstone of Alzheimer’s research, as identifying these indicators could lead to timely diagnosis and intervention. Biomarkers can provide early signs of the disease, allowing for treatment plans to be initiated before significant cognitive decline occurs. Through the lens of microglial research, significant strides have been made in discovering potential biomarkers associated with neuroinflammation and abnormal synaptic pruning, which are hallmarks of Alzheimer’s. As researchers like Beth Stevens focus on understanding the relationship between microglia and synaptic health, the identification of specific biomarkers linked to microglial dysfunction becomes increasingly plausible.
Additionally, advancements in biomarker discovery have implications for not only diagnosing Alzheimer’s but also for monitoring disease progression and treatment efficacy. If successful, these biomarkers can guide therapeutic strategies and foster personalized medicine approaches in caring for individuals with Alzheimer’s disease. The integration of microglial research into biomarker development highlights the importance of interdisciplinary studies in the realm of neurodegenerative diseases. As the field continues to evolve, the promise of effective biomarkers holds the potential to change how clinicians approach the management of Alzheimer’s and enhance patient outcomes significantly.
Microglial Cells: The Brain’s First Line of Defense
Microglial cells serve as the brain’s primary defense mechanism against disease and injury, acting as the brain’s immune system. Their ability to detect and respond to pathological changes is vital for maintaining neural homeostasis. Research led by Beth Stevens has shed light on the various functions of microglia, from surveillance and debris clearance to neuroprotection and modulation of neuroinflammatory responses. By understanding how microglial cells operate under normal and pathological conditions, researchers can better comprehend the onset of neurodegenerative diseases such as Alzheimer’s and develop strategies to bolster brain health.
In the face of Alzheimer’s, microglial cells perform a dual role; while they help clear plaques and debris, dysregulation of their activity can also contribute to disease progression. If microglia overreact to minimal signals of damage, this can lead to chronic inflammation, a significant factor in the deterioration of cognitive function associated with Alzheimer’s. Therefore, ensuring that these cells function properly is critical for not only neuroprotection but also for preventing the adverse outcomes associated with neurodegenerative diseases. Future therapies might focus on correcting microglial dysfunction as a means of protecting brain health and combating Alzheimer’s.
The Interconnection Between Synaptic Health and Neurodevelopment
The interplay between synaptic health and neurodevelopment is a crucial area of investigation in neuroscience, particularly concerning the roles of microglial cells. These cells not only facilitate the development of neural circuits during early life but also maintain synaptic integrity throughout adulthood. Abnormal microglial pruning can disrupt synaptic function, leading to various neurodevelopmental and neurodegenerative disorders, including Alzheimer’s disease. The work of researchers like Beth Stevens highlights the necessity of exploring how microglial interactions influence both normal and pathological states of brain function.
Understanding the links between synaptic health and microglial activity may illuminate the mechanisms underlying cognitive decline in Alzheimer’s disease. For example, the loss of synapses is a significant predictor of cognitive impairment in adults. As we continue to unravel the complexities of neurodevelopment and the role of microglia, it becomes increasingly apparent that maintaining synaptic health is essential for preventing neurodegeneration. Advancements in this research area hold the promise of identifying new therapeutic targets that can support cognitive health across the lifespan.
Challenges and Future Directions in Alzheimer’s Research
Despite the advancements made in Alzheimer’s research, significant challenges remain in fully understanding and effectively treating the disease. While the contributions of microglial research have provided valuable insights, the complexity of Alzheimer’s pathology requires a multifaceted approach. Researchers must integrate knowledge from various disciplines, including genetics, neurobiology, and environmental factors, to develop comprehensive models of the disease. The continued support of initiatives that foster interdisciplinary collaboration is vital for addressing the unanswered questions surrounding Alzheimer’s.
Looking forward, the focus on early intervention strategies may reshape how Alzheimer’s is approached in clinical settings. By identifying specific biomarkers and understanding microglial roles in synaptic health, future therapies could be designed to mitigate the onset of cognitive decline. This proactive approach reflects a shift from reactive treatment to preventative care, emphasizing the need for sustained investment in research. As scientists continue to unravel the mysteries of Alzheimer’s disease, the hope is to convert scientific knowledge into real-world benefits that ultimately improve the lives of millions.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s disease research?
Microglial cells are essential components of the brain’s immune system and play a crucial role in Alzheimer’s disease research. They help monitor brain health by removing dead or damaged cells and pruning synapses. However, abnormal microglial activity is linked to neurodegenerative diseases, including Alzheimer’s, which has led researchers like Beth Stevens to identify potential biomarkers and therapeutic targets.
How does microglial research contribute to our understanding of neurodegenerative diseases?
Microglial research significantly enhances our understanding of neurodegenerative diseases by revealing how these immune cells interact with neuronal systems. Studies have shown that dysfunction in microglial activity can lead to improper synaptic pruning, which is associated with diseases like Alzheimer’s and Huntington’s. This research is pivotal for developing new treatment strategies.
What are some recent scientific discoveries in microglial research?
Recent scientific discoveries in microglial research include insights into their role in synaptic pruning during normal brain function and the pathological effects they have in neurodegenerative diseases like Alzheimer’s. These findings, propelled by curiosity-driven studies, are shaping new approaches to detect and treat such disorders.
Why is funding important for microglial research in Alzheimer’s disease?
Funding is critical for microglial research as it supports the basic science necessary for understanding the underlying mechanisms of Alzheimer’s disease. As highlighted by researchers like Beth Stevens, federal funding from organizations like the NIH is essential for pursuing groundbreaking studies that lead to the development of new therapeutic interventions and biomarkers.
How does microglial dysfunction affect synaptic health in neurodegenerative diseases?
Microglial dysfunction can lead to improper synaptic pruning, which negatively impacts synaptic health and contributes to neurodegenerative diseases such as Alzheimer’s. This abnormal activity can result in the loss of important neural connections, exacerbating the cognitive decline associated with these conditions.
What implications do current microglial research findings have for future Alzheimer’s therapies?
Current findings in microglial research have significant implications for future Alzheimer’s therapies. By understanding how microglia contribute to synaptic health and disease progression, researchers can develop targeted treatments aimed at restoring normal microglial function, potentially slowing down or altering the course of Alzheimer’s disease.
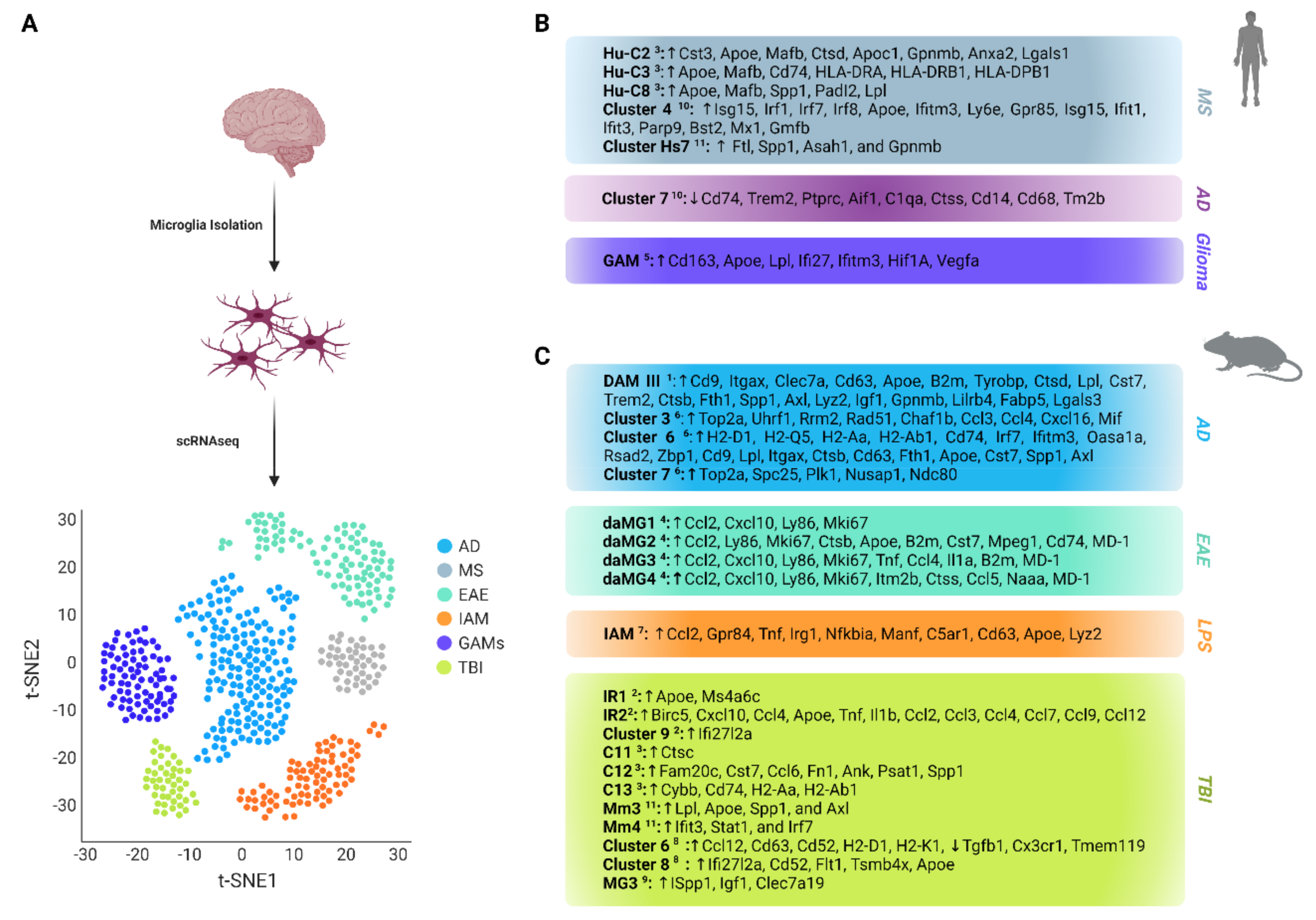
What is the significance of using animal models in microglial research for neurodegenerative diseases?
Animal models are critical in microglial research as they allow scientists to investigate the brain’s immune responses in a controlled environment. Through these models, researchers can study the intricate behaviors of microglia in relation to neurodegenerative diseases, providing insights that are difficult to obtain directly from human subjects.
How does basic science facilitate advancements in microglial research related to Alzheimer’s?
Basic science plays a vital role in facilitating advancements in microglial research by providing foundational knowledge about brain immune responses. This curiosity-driven approach allows researchers to uncover novel insights into the cellular mechanisms that underlie Alzheimer’s disease, paving the way for innovative diagnostic and therapeutic strategies.
| Key Area | Details |
|---|---|
| Researcher | Beth Stevens, NIH-supported investigator at Boston Children’s Hospital and Harvard. |
| Focus Area | Microglial cells and their role in brain immunity and health. |
| Key Findings | Microglia prune synapses and remove damaged cells; abnormal pruning linked to Alzheimer’s and other disorders. |
| Impact | Research lays groundwork for new biomarkers and therapies for neurodegenerative diseases. |
| Funding | Research supported by federal funding, primarily from NIH. |
| Quote | “Our microglial research is a prime example of an immune-related pathway and cell type that we could never have advanced without foundational and curiosity-driven research.” Beth Stevens. |
Summary
Microglial research is transforming our understanding of brain health and disease. Researchers like Beth Stevens are uncovering the pivotal role of microglial cells in maintaining neural integrity and their impact on conditions such as Alzheimer’s disease. Stevens’ insights into the dual nature of microglial function—as protectors and potential contributors to neurodegenerative disorders—are paving the way for innovative approaches to treatment and prevention. This work underscores the importance of foundational research, funded by institutions like the NIH, in enabling significant advancements in neuroscience.